ABN in a nutshell
May 21, 2024
ABN in a nutshell
Michelle Kirk
Manager, Revenue Cycle CPC, CPCO, COCAS
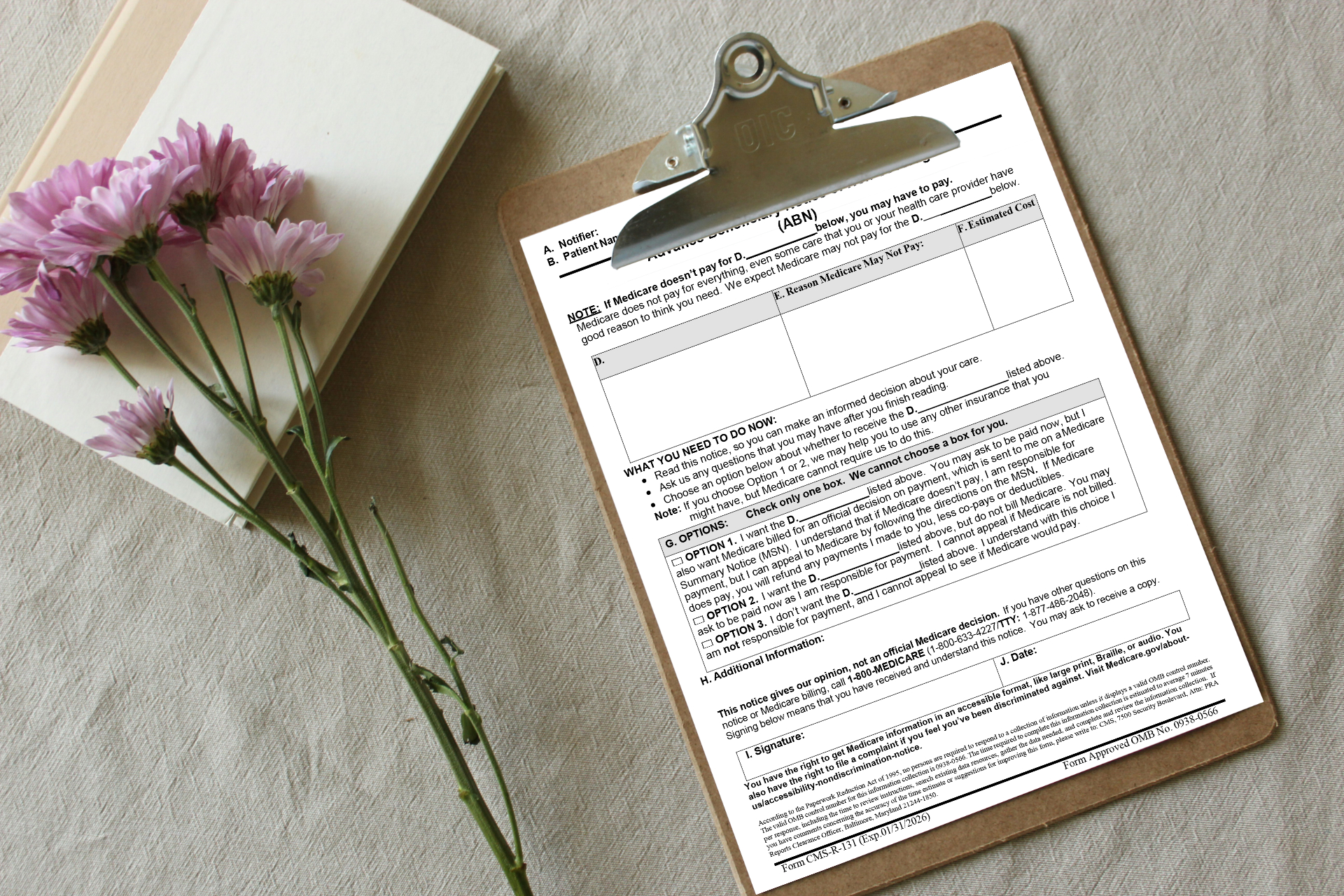
An Advance Beneficiary Notice (ABN) is a written notice from Medicare that informs a patient that Medicare may not cover certain services or items aka Advance Beneficiary Notice of Noncoverage. The patient is informed before receiving the service with details on why it might be denied. This allows the patient to choose whether to proceed and pay for it themselves if denied payment by Medicare .
Medical Necessity of Tests Ordered- Laboratories must make sure that they should only bill for services that are considered reasonable and necessary. Medicare could refuse to pay for tests that do not meet their criteria (i.e., done for screening purposes) or lack proper documentation. Patients may have to pay for these tests themselves if they are not covered.
Additional supporting documentation is required when clinical circumstances do not support medical necessity. Medical records, clinical studies, etc., must be provided to demonstrate why the service billed is reasonable and necessary. Medicare and private payers limit coverage to certain conditions by assigning procedure codes to covered diagnosis codes. Patients should receive an Advanced Beneficiary Notice (ABN) for services that are excluded through a local or national coverage determination.
Modifiers are used to show the condition of an advanced beneficiary notice (ABN) while sending claims to Medicare. An ABN is utilized to notify a recipient of their financial responsibility, right to appeal, and safeguards within the fee-for-service (FFS) Medicare program. Providers and suppliers must ensure they utilize the correct modifier when submitting claims to specify the presence or absence of an ABN signed by the beneficiary.
Modifiers associated with ABN use.
|
Modifier |
When to use the Modifier |
|
GA |
modifier should be used when physicians, practitioners, or suppliers want to indicate that they expect Blue Cross of Idaho will deny a service as not reasonable and necessary and they do have an Advanced Beneficiary Notice (ABN) signed by the member. |
|
GX |
modifier should be used when physicians, practitioners, or suppliers want to indicate that they issued a voluntary ABN. Providers can bill the GX modifier on the same claim line as the GY modifier. |
|
GY |
modifier should be used when physicians, practitioners, or suppliers want to indicate that the item or service is statutorily non-covered or is not a Medicare-covered benefit. |
|
GZ |
modifier should be used when physicians, practitioners, or suppliers want to indicate that they expect that Blue Cross of Idaho will deny an item or service as not reasonable and necessary and they have not had an advance beneficiary notification (ABN) signed by the member. |