Denial Management
Why Choose Revenulytics as your Denial Management Partner?
Our team pinpoints the underlying reasons for your claim rejections and, when applicable, composes compelling appeal letters to assertively reclaim funds for any that are reversed. Our specialists in denial management then offer guidance and analytical insights on patterns to enhance procedures, thereby diminishing and forestalling the total frequency of claim refusals over time.
Why choose our medical coders?
What Is Denial Management?
Denial management is an important aspect of healthcare revenue cycle management that involves the identification, tracking, and resolution of claim denials. Denial management is critical to the financial success of any healthcare organization as it helps to ensure that claims are paid accurately and timely. The process involves analyzing the reasons for claim denials, taking appropriate corrective actions, and implementing strategies to prevent future denials.
At its core, denial management is about understanding why claims are denied and taking steps to avoid those denials in the future. There are many reasons why claims may be denied, including coding errors, incorrect patient information, lack of documentation, and issues with eligibility or pre-authorization. Identifying the root causes of these denials is essential to creating effective solutions.
One key component of denial management is the use of analytics and data to track and analyze denial trends. By analyzing data related to claim denials, organizations can identify patterns and trends that may be contributing to denials. This information can be used to create targeted strategies to address specific denial issues and improve overall revenue cycle performance.
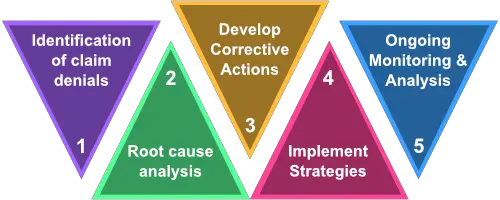
Effective denial management requires a comprehensive approach that includes the following key steps:
- Identification and analysis of claim denials
- Root cause analysis to identify reasons for denials
- Development of corrective actions to address denial issues
- Implementation of strategies to prevent future denials
- Ongoing monitoring and analysis to ensure continued success
Denial management is an ongoing process that requires dedication and attention to detail. By taking a proactive approach to denial management, healthcare organizations can improve their revenue cycle performance and ensure that claims are paid accurately and timely.